Who is More Prone to DVT, and How to Manage the Symptoms of DVT?
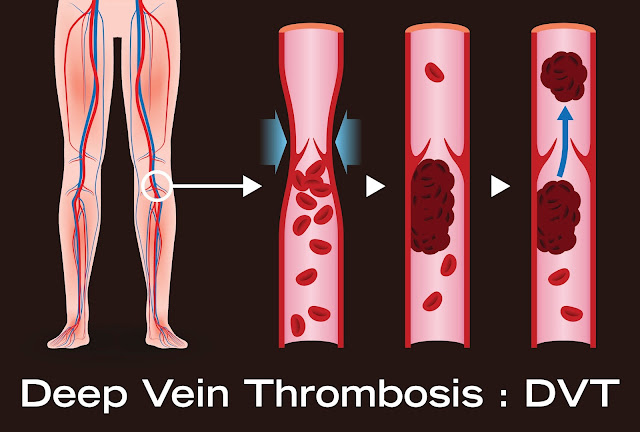
Deep Vein Thrombosis (DVT) is a condition characterised by the formation of blood clots in the deep veins, typically in the lower legs. It can have serious implications if left untreated, including the risk of pulmonary embolism. Certain individuals are more prone to developing DVT due to various risk factors. In this article, we will delve into the common causes and symptoms of DVT, and also discuss who is at a higher risk for this disease. Moreover, we will explore the various treatments available and discuss preventative measures that can be taken to mitigate the risk of developing DVT. By understanding the causes, recognising the symptoms, and adopting preventive strategies, individuals can take proactive steps towards maintaining their vascular health.
Who is more prone to DVT?
Certain individuals are more prone to developing Deep Vein Thrombosis (DVT) due to various risk factors. Here are some factors that can increase the likelihood of developing DVT:
-
Prolonged immobility
Extended periods of immobility can hinder the blood flow in the veins, increasing the risk of clot formation. Situations such as long-haul flights, where individuals are seated for long durations without much leg movement, can contribute to DVT. Similarly, prolonged bed rest or being confined to a wheelchair can also increase the risk. The lack of movement reduces the contraction of muscles in the legs that help pump blood back to the heart, allowing blood to pool and potentially form clots.
-
Surgery and hospitalisation
Major surgeries, particularly those involving the lower extremities or the pelvis, can increase the risk of DVT. Surgical procedures may damage blood vessels, trigger an inflammatory response, or require periods of immobility during recovery. Additionally, being hospitalised for any reason can contribute to immobility and increase the likelihood of clot formation. Healthcare providers take precautions to mitigate this risk by implementing strategies like early mobilisation, compression stockings, and blood-thinning medications when appropriate.
-
Age
The risk of DVT generally increases with age. As individuals get older, the veins and valves in the legs may become less efficient in returning blood to the heart, making them more prone to clot formation. Additionally, older adults may have other underlying health conditions or lifestyle factors that further contribute to DVT risk.
-
Obesity
Excess weight puts additional pressure on the veins, making it more difficult for blood to circulate properly. The impaired blood flow, combined with potential inflammation caused by obesity, increases the risk of clot formation. Furthermore, obesity is often associated with other health conditions such as diabetes or hypertension, which can further elevate the risk of DVT.
-
Pregnancy and the postpartum period
During pregnancy, various changes occur in a woman's body that can increase the risk of DVT. Hormonal changes, increased pressure on the veins in the pelvis due to the growing uterus, and reduced blood flow in the legs can all contribute to the development of blood clots. The risk remains elevated for a period after giving birth due to factors like reduced mobility and potential damage to blood vessels during childbirth. Pregnant women need to be aware of these risks and follow preventive measures recommended by healthcare professionals.
-
Previous history of DVT or pulmonary embolism
Individuals who have previously experienced DVT or pulmonary embolism are at a higher risk of recurrence. Having a history of blood clot formation indicates a propensity for clotting, and precautions should be taken to prevent future episodes. Healthcare providers may prescribe long-term anticoagulant medication or recommend preventive measures to minimise the risk of recurrence.
-
Cancer and its treatments
Certain types of cancer, particularly those that affect the blood or have a tendency to spread, can increase the risk of DVT. Additionally, cancer treatments such as chemotherapy or hormone therapy may interfere with the normal clotting process and elevate the risk. Patients with cancer should work closely with their healthcare team to manage the risk of DVT during treatment.
-
Inherited or acquired blood clotting disorders
Some individuals may have inherited or acquired conditions that affect the blood's clotting ability, making them more susceptible to DVT. Inherited disorders like Factor V Leiden mutation or deficiencies in proteins involved in the clotting process can increase the risk. Acquired conditions, such as antiphospholipid syndrome or certain autoimmune disorders, can also contribute to an increased tendency for blood clot formation.
Common symptoms of DVT
Here are the common symptoms of Deep Vein Thrombosis (DVT) presented in bullet points:
- Swelling may appear in the affected foot, ankle, and leg
- Pain or tenderness in the leg, often starting in the calf and sometimes described as a cramp or soreness
- The affected area becomes warmth and red
- Skin discolouration, such as turning pale or bluish
- Visible veins
- Increased pain when standing or walking
- Heavy ache or throbbing sensation in the leg
- Leg fatigue or heaviness
- Skin that feels unusually warm to the touch
How to Manage the Symptoms of DVT?
Managing the symptoms of Deep Vein Thrombosis (DVT) is an important aspect of the overall treatment plan. Here are some strategies to help manage the symptoms associated with DVT:
-
Medical treatment
The primary goal of medical treatment for DVT is to prevent the clot from growing larger, reduce the risk of complications, and promote the body's natural clot-dissolving mechanisms. Healthcare providers often prescribe anticoagulant medications, such as heparin or warfarin, to thin the blood and prevent further clot formation. It is crucial to strictly follow the prescribed dosage and schedule as directed by the healthcare professional.
-
Compression therapy
Wearing compression stockings or garments can help alleviate symptoms of DVT by promoting blood flow in the affected leg. Compression stockings apply gentle pressure to the legs, helping to prevent blood from pooling and reducing swelling. These specialised stockings should be properly fitted and worn as recommended by healthcare professionals.
-
Elevation of the affected limb
Elevating the affected leg can assist in reducing swelling and pain. Prop up the leg on pillows or cushions to raise it above the level of the heart. This position helps facilitate venous blood flow and reduces pressure in the affected veins.
-
Pain management
Over-the-counter pain relievers, such as acetaminophen (Tylenol), may help manage mild to moderate pain associated with DVT. However, it is essential to consult with a healthcare professional before taking any medications, as certain pain medications (such as nonsteroidal anti-inflammatory drugs or NSAIDs) may increase the risk of bleeding in individuals taking anticoagulant medications.
-
Regular physical activity
Engaging in regular physical activity, as advised by healthcare professionals, can improve blood circulation and alleviate symptoms of DVT. Walking, leg exercises, and gentle movements can help prevent blood from pooling and encourage healthy circulation. It is important to consult with a healthcare professional before starting any exercise regimen to ensure it is safe and appropriate for your specific condition.



Comments
Post a Comment